I was still spotting the next morning, so we decided to go to the emergency room. It was actually my first ER visit ever in Israel, and the third one of my life overall, and I was surprised with how efficient and professional they were. Thank G-d the ultrasound showed 2 heartbeats, though the resolution on the machine was pretty poor, so we weren't able to see much more than that. It was such a huge relief - we were up the whole night Friday, trying to prepare ourselves for horrible news.
I had ketones in my pee when we were at the ER, so I got a few liters of fluid and IV Zofran. In general, the morning sickness has been pretty miserable, but it is what I would expect with twins, and honestly, it seems like a small price to pay as long as I can still get enough fluids and nutrients to keep the babies going strong. I have had a few particularly horrible days, but I seem to be in better shape now that I am on a consistent schedule with Zofran. I have it every morning first thing with a popsicle in bed and it seems to help start things off on the right foot.
Today, since it was the weekend, I procrastinated a bit on taking the Zofran and I really paid for it. Luckily, Y has brought home all of the supplies to give me IV fluids at home, which has been a great set-up. He has saved us many trips to the urgent care clinic or ER by giving me fluids at home, and it is much more comfortable to be in my bed than somewhere else.
Y and I have both been reading Dr. Luke's book When You're Expecting Twins, Triplets, or Quads and as a result, we are realizing how important proper weight gain is for a multiples pregnancy. Dr. Luke's main schtick is that you can maximize your chances of a positive multiples pregnancy outcome with proper nutrition and also by gaining a lot more weight than with a singleton pregnancy and than conventional wisdom would dictate.
I do believe that this is something worth focusing on since I feel like it is one of the very few factors I have control over in determining our pregnancy outcome. Honestly, it is quite daunting though, since she emphasizes the importance of weight gain early in pregnancy and I am having such a difficult time just trying to eat what I usually do, never mind 1000+ calories more, because of the morning sickness. Still, I am really going to try to step it up with the eating.
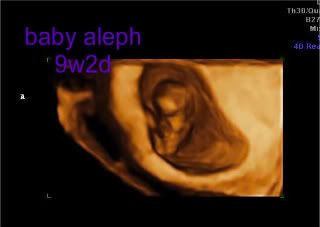
After the bleeding episode, we had a routine ultrasound and appointment with our RE. Initially, both babies were measuring 4 days behind based on CRL. As of last week, baby aleph was measuring 1 day behind and baby bet was measuring 2 days behind, so I am feeling pretty good about their progress. The only thing that is a little strange is that baby bet's gestational sac has been measuring behind. In ultrasound pictures, you can definitely see that baby bet has less room in his/her sac than baby aleph, whose sac is more consistent with his/her gestational age. Hopefully this is meaningless.
My fibroids also have been growing quite a bit, and the ultrasound tech pointed out one that is adjacent to baby bet. Hopefully, the fibroids will behave themselves and the babies will be unimpeded with all of the space they need to grow and thrive. The source of the bleeding was never identified, though everyone did say that bleeding is more common in pregnancies with multiples. I spent most of last week at home on modified bedrest as a precaution to minimize the chance that the bleeding would start again, and thankfully, I haven't seen anything since last weekend.
Our next ultrasound is the NT scan, which will be on January 16 at 12w3d. I am excited for that to be done and over with and I pray that it goes well - then maybe we will consider beginning to share our pregnancy. I have an appointment with a high-risk ob/gyn a few days after the NT scan and then a hematology appointment about a week after that.
In other news, I bought a home doppler online a few days ago and it should arrive very soon. I paid a small fortune in shipping since the 2 major options seemed to be ordering it from the U.S. (but with only one international shipping method which is express and very pricey) or via eBay from China (but with only one international shipping method which is 'economy' and could take 4 weeks). I decided to take the hit and order it from the U.S. with express delivery :)
I think that is pretty much all that is new around here - this was quite a long update. I still think about how fragile all of this every single day. As I am slowly becoming a little less anxious about miscarriage, though, I am also feeling more and more grateful to be where we are right now. I really hope and pray I will hold 2 healthy babies in my arms in 2012 - it will be the fulfillment of my wildest dreams if this all pans out. To my buddies still in waiting, I pray that 2012 will bring the fulfillment of your wildest dreams, too!
Lastly, here are a few pics from our last ultrasound at 9w2d: